Cryptococcus
CASE 1
• A 34 year old woman received her third course of chemotherapy for Hodgkin's disease one month ago. Since then, she has had a increasing occipital headache and stiff neck. She began having mild, low grade fever and sweats over the same period.
• On physical examination, she was afebrile. There was mild neck stiffness with discomfort on anteflexion. The resst of the neurological examination was normal.
• A complete blood count was remarkable for a WBC count of 2,300 with 42% neutrophils. A serum cryptococcal antigen test was negative.
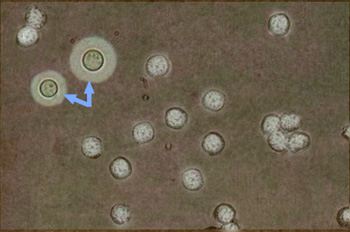
• Because the patient had received chemotherapy, steroids, and had been neutropenic, it was decided to perfrom a lumbar puncture to investigate the cause of her headache. The fluid was clear, and the opening pressure was normal. There were 350 WBCs, all mononuclear cells. The CSF glucose was one-third of the lower limit of normal; and the CSF protein was double the upper limit of normal. Bacterial culture was negative, but a concentrated preparation of CSF, which was negatively-stained with India ink, showed many leukocytes and a rare structure as shown in the figure by the blue arrows and identified as Cryptococcus neoformans. A cryptococcal antigen test on the CSF was positive at a titre of 1:5120.
• The patient was treated with an extended course of high-dose fluconazole, and her symptoms gradually resolved. The initial CSF sample eventually turned positive for Cryptococcus on a fungal culture. A repeat lumbar puncture 6 weeks later revealed only 12 WBCs/mm3 and a normal CSF glucose. The culture from the repeat lumbar puncture was negative, although a cryptococcal antigen test on the fluid was positive at 1:64.
Questions:
1. How was cryptococcus acquired? What was the portal of entry?
2. How did it get to the meninges?
3. What is cryptococcal antigen, and why was it absent in the serum sample but present in the CSF sample in large amounts?
4. What is the unstained substance that creates a halo around the smaller yeast cells on the India Ink stain?
5. How do you account for the CSF WBC count? the low CSF glucose? the high CSF protein?
6. What other common form of chronic meningitis in Ghana may present with similar symptoms and with identical CSF cell counts, glucose and protein?
6. Are you concerned that the CSF cryptococcal antigen is still positive after 6 weeks of treatment?
CASE 2
• A 43 year old man with advanced HIV comes to the hospital with increasing fever and severe headache of 8 days duration. The patient has been having increasing chills and sweats during the past week. A malaria smear is negative. Examination reveals a stiff neck. By the time the patient is admitted to the hospital, he complains that he has the worst headache of his life.
• The patient has a temperature of 39.5 degrees. He has nuchal rigidity. He is partially disoriented (unable to remember the day of the week or the month).
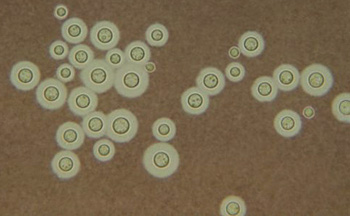
• A lumbar puncture is performed. The fluid is slightly turbid and spurts from the spinal needle when it is accessed. There are no WBC cells, the CSF glucose is normal, and the CSF protein is mildly elevated. Cryptococcal antigen testing of the CSF is positive at a titre of >1:102,400. Serum cryptococcal antigen is also positive at 1:32. The appearance of the concentrated CSF with Indai ink is shown below:
• The patient is treated with intravenous amphotericin B for one week and then switched to high-dose oral fluconazole. He undergoes lumbar puncture daily for the first week of therapy with removal of 20-40 cc of spinal fluid, each tap resulting in a dramatic decrease in his headache.
Questions:
1. Which features of this case distinguish it from the previous one? Why are there differences?
2. What is the meaning of a negative WBC count in the spinal fluid?
3. What is causing the patient's headache? How has this infection caused the spinal fluid pressure to increase?
4. Note that the serum cryptococcal antigen is positive. Knowing this could you avoid doing a lumbar puncture altogether and simply treated the patient for cryptococcal meningitis?
5. How long will this patient have to be treated?