Bacteroides and other Gram-negative Obligate Anaerobes
CASE 1
• An 18-year-old college freshman comes to the hospital with diffuse abdominal pain, diarrhea, and nausea. Pain is localized to the right side of the abdomen.
• On physical examination, she has tenderness with rebound over the right lower quadrant of the abdomen. She is treated with a 1st generation cephalosporin on the way to the surgical theatre where a ruptured appendix is removed. A blood culture was obtained.
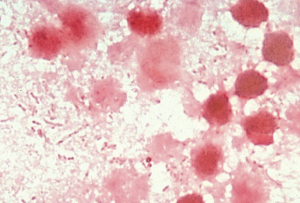
• At surgery, a Gram stain and culture of the peritoneum are obtained. The Gram stain is shows mixed Gram-negative flora (below). The culture grows E. coli and other typical fecal bacteria.
• On the second post-operative day, her temperature rises to 38.6°C. Her blood culture obtained prior to surgery grows E. coli, sensitive to the cephalosporin that received. She completed a 7-day course of cefazolin and improved.
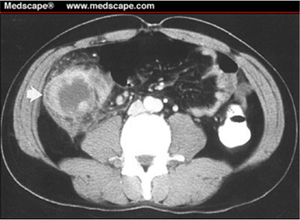
• However, 36 hours later, her temperature again rose to 38.8°C and she felt diffuse pain over the site of the appendectomy. A CT scan of her abdomen revealed a retroperitoneal abscess (see the white arrow in the CT scan below). The abscess was drained with a catheter and an anaerobic culture of the abscess fluid grew Bacteroides fragilis and a few Eubacteria.
Questions:
1. How did the two episodes of her disease differ with regard to pathogenesis and to the kind of bacteria involved?
2. Why did B. fragilis survive the first course of antibiotic treatment?
3. Was she treated properlyafter the first surgery?
4. What could have been done to lessen the likelihood of abscess formation?
5. How does B. fragilis synergize with intestinal facultative bacteria (e.g., E. coli) to facilitate intra-abdominal abscess formation?
6. Which specific feature of Bacteroides fragilis make it especially able to survive outside the colon and to facilitate abscesses?
CASE 2
• A 53 year old hypertensive man is admitted to the hospital after suffering a hemorrhagic stroke with a right hemiplegia (paralyzed right arm and leg). He is obtunded (i.e., arousable with stimulation, but otherwise asleep). His breathing is deep and his cough reflex is depressed.
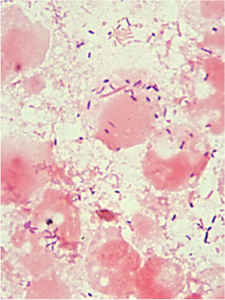
• On the 4th hospital day, he develops a fever to 38.4 degrees and his respirations are noted to have increased from 20 per minute to 30. He is given oxygen through a nasal catheter. A chest xray is taken and it reveals an infiltrate in the right lower lobe(see below left). A Gram stain shows mixed flora (see below right). A culture of a tracheal aspirate grew normal oral flora.

• A diagnosis of aspiration pneumonia is made and the patient is placed on antibiotic therapy with activity against oral flora and obligate anaerobes. He fever resolves promptly, and he recovers his respiratory function byt the end of the week.
Questions:
1. Why did this patient aspirate? What did he aspirate in the lung?
2. Why was the right lower lobe involved?
3. List some oral bacteria that might be present in the lung?
4. List some oral or intestinal obligate anaerobic bacteria that might be present in the lung?
CASE 3
• A 22 year old male who recently had an prolonged episode of pharyngitis now presents with high fever, and exquisite pain, tenderness and swelling of his left neck for 2 days. This morning, he developed sharp pain in the left lower chest with deep breathing.
• A chest xray shows changes consistent with a pulmonary infarction, likely associated with mobilization of a venous blood clot to the lungs and obstruction of a pulmonary artery branch. A CT scan of the neck revealed the source of the blood clot in the left external jugular vein (note the failure of the intravenous contrast to whiten that particular vessel).
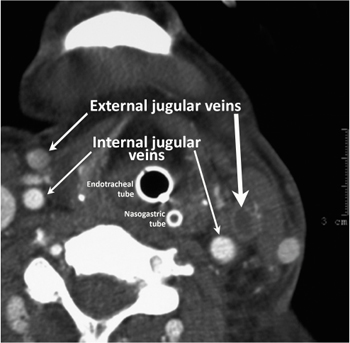
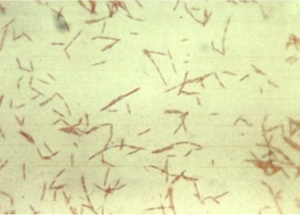
• Based on these findings, a clinical diagnosis of post-anginal sepsis (Lemierre's syndrome, or septic thrombophlebitis due to Fusobacterium) was made. Treatment with an antibiotic active against fusobacteria was initiated. A blood culture later became positive for the obligate anaerobe, Fusobacterium necrophorum, so named because of the tapering ends of the long bacilli.
Questions:
1. What was the likely source of this potentially dangerous anaerobic organism?
2. Why did this rare complication occur in this particular patient?