Nocardia
CASE 1
• A 70 year old man with chronic lymphocytic leukemia has had a pulmonary infiltrate in the right mid lung field with fevers and night sweats for the past 3 weeks. Sequential treatments with ceftriaxone and ciprofloxacin have not been helpful. Instead of improvement, there is now a cavity developing at the center of the infiltrate, and there are two new enlarged and tender lymph nodes in the right axilla. In addition, the patient is experiencing weakness of the left hand.
• To make a diagnosis, one of the lymph nodes is removed. Shortly after this procedure, the patient has a grand mal seizure..
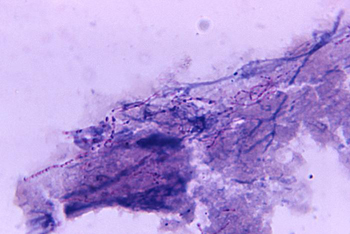
• A touch preparation of node is prepared on a slide an stained with a Gram stain and a modification of the acid-fast technique. The Gram stain shows slender, branching Gram-positive rods. The modified acid-fast stain shows the same bacteria, suggesting that they are Nocardia spp.
• Treatment is begun once again with sulfamethoxasole-trimethoprim in high dose, and the symptoms and signs resolve slowly over the next 3 months.
Questions:
1. Which species of Nocardia is likely to have caused this disease?
2. Why did this patient develop pulmonary Nocardia infection?
3. How did the organism enter his lungs? Was the patient colonized with the organism in the mouth or upper respiratory tract?
4. Why did the patient experience weakness of the hand and a new seizure?
5. Why is it important to distinguish Nocardia infections from Actinomyces infections? What clinical features distinguish these infections? Which laboratory tests distinguish them?
6. How would you culture the lymph node if you wished to isolate the bacteria in the lab?