Pneumococcus
CASE 1
• A 58 year old man with a history of chronic bronchitis awakens at 2:00am with a rigorous, shaking chill. This is followed promptly by the development of sharp pain over the left lateral chest and a productive cough. The patient begins to produce yellow sputum with streaks of blood. As the symptoms worsen, and the chills continue, the patient comes to the Emergency Department at the Komfo Anokye Teaching Hospital for treatment.
• At presentation, he appears ill and in pain with coughing. A chest xray is obtained and show the follwoing changes (see below). For comparison, the panel to the right shows the position of the major organs of the chest superimposed on the xray. The physician in charge recognizes pulmonary infiltrates (which appear white in the usually black lung fields) in the right lower and left upper and lower lobes. There is also a pleural effusion (fluid in the pleural space) on the left.

.jpg)
• A Gram-stain of the patient's sputum is obtained (below). The sputum is cultured, and a blood sample is also taken for culture.
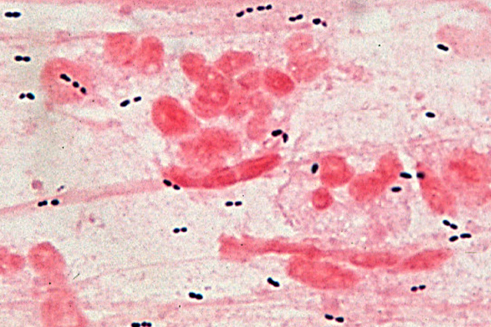
• The blood culture grew Streptococcus pneumoniae 36 hours later. The sputum culture remained negative.
Questions:
1. What factors predispose this patient to the development of pneumococcal pneumonia?
2. Why does the patient having chest pain and a pleural effusion?
3. What is the principle virulence factor of this organism that prevents it from being eliminated by the immune system?
4. If the patient were to recover from this illness without treatment, which components of his immune system will eventually combine to clear the bacteria?
5. What is the significance of serotyping of the pneumococci? How does serotyping influence the possibility of reinfection and the composition of vaccines?
6. Is the Gram stain diagnostic of this disease?
7. Why was the sputum culture negative and the blood culture positive? Do all patients with pneumococcal pneumonia have positive blood cultures? What does the presence of pneumococci in the blood suggest?
CASE 2
• The patient described above is hospitalized and treated with the macrolide antibiotic, azithromycin. After two days in the hospital, the patient has become disoriented and his fever has increased. Re-examination reveals that his neck is now stiff when trying to passively lift his head from the pillow.
• A lumbar puncture is performed and yields 5cc of slightly turbid cerebrospinal fluid. The leukocytes count of the fluid is 350/mm3 with 95% of the cells being neutrophils (normal CSF leukocyte count is <10/mm3 with no neutrophils). A Gram stain of the fluid shows rare Gram-positive diplococci.
• The treatment is changed to high-dose ceftriaxone, and the patient begins to improve gradually. He is discharged to home after receiving pneumococcal vaccine.
Questions:
1. Does pneumococcus cause meningitis? If so, how do you think the organism got to the meninges in this case? Why was the antibiotic therapy ineffective in preventing this complication?
2. If the patient had infection with pneumococcus, is it sensible or necessary to give him pneumococcal vaccine before he leaves the hospital?